Dementia Fall Risk - An Overview
Wiki Article
The Basic Principles Of Dementia Fall Risk
Table of ContentsThe 4-Minute Rule for Dementia Fall RiskRumored Buzz on Dementia Fall RiskUnknown Facts About Dementia Fall RiskThe Buzz on Dementia Fall Risk
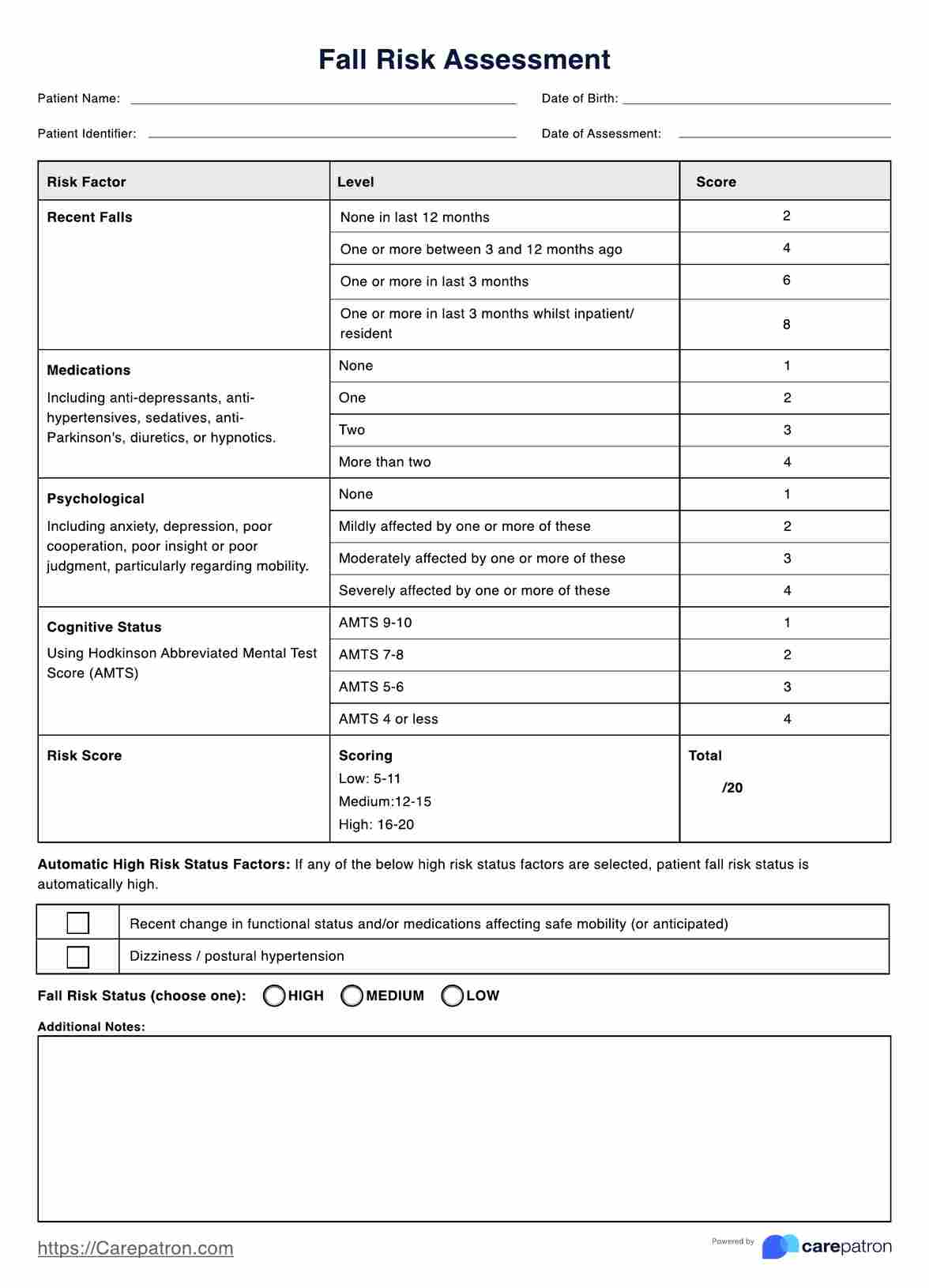
A loss danger assessment checks to see how most likely it is that you will drop. The assessment generally includes: This includes a series of concerns regarding your general wellness and if you've had previous falls or issues with equilibrium, standing, and/or walking.Interventions are referrals that may minimize your risk of falling. STEADI consists of 3 actions: you for your danger of falling for your threat variables that can be improved to try to protect against drops (for instance, equilibrium issues, impaired vision) to minimize your risk of falling by using efficient approaches (for instance, providing education and learning and resources), you may be asked several inquiries consisting of: Have you dropped in the previous year? Are you fretted regarding falling?
You'll sit down again. Your provider will check how lengthy it takes you to do this. If it takes you 12 secs or more, it might indicate you are at higher danger for a fall. This examination checks stamina and balance. You'll sit in a chair with your arms went across over your upper body.
Move one foot midway forward, so the instep is touching the huge toe of your other foot. Relocate one foot completely in front of the other, so the toes are touching the heel of your various other foot.
More About Dementia Fall Risk
The majority of falls take place as a result of multiple contributing variables; as a result, managing the risk of dropping starts with identifying the factors that add to drop risk - Dementia Fall Risk. Several of the most appropriate danger variables include: Background of prior fallsChronic clinical conditionsAcute illnessImpaired gait and equilibrium, reduced extremity weaknessCognitive impairmentChanges in visionCertain high-risk medicines and polypharmacyEnvironmental elements can also enhance the danger for falls, including: Insufficient lightingUneven or harmed flooringWet or unsafe floorsMissing or harmed hand rails and grab barsDamaged or improperly fitted devices, such as beds, wheelchairs, or walkersImproper use of assistive devicesInadequate guidance of individuals living in the NF, including those who exhibit hostile behaviorsA effective fall risk management program calls for an extensive clinical assessment, with input from all members of the interdisciplinary team
The treatment strategy must additionally consist of treatments that are system-based, such as those that advertise a safe environment (ideal illumination, handrails, get hold of bars, and so on). The efficiency of the interventions should be examined occasionally, and the treatment plan modified as necessary to show modifications in the loss danger analysis. Executing a fall danger administration system using evidence-based finest practice can decrease the frequency of falls in the NF, while limiting the capacity for fall-related injuries.
The Ultimate Guide To Dementia Fall Risk
The AGS/BGS standard advises evaluating all adults matured 65 years and older for fall danger each year. This screening includes asking clients whether they have fallen 2 or more times in the previous year or sought clinical focus for a loss, or, if they have actually not fallen, whether they really feel unsteady when strolling.People that have actually fallen as soon as without injury should have their equilibrium and gait reviewed; those with gait or equilibrium problems ought to obtain extra analysis. A history of 1 loss without injury and without stride or great post to read equilibrium troubles does not necessitate more analysis beyond ongoing annual loss danger screening. Dementia Fall Risk. A fall threat assessment is required as part of the Welcome to Medicare examination

Dementia Fall Risk - Questions
Documenting a falls history is one of the top quality indicators for loss prevention and administration. copyright medications in certain are independent predictors of drops.Postural hypotension can often be reduced by see here now decreasing the dosage of blood pressurelowering drugs and/or stopping medications that have orthostatic hypotension as a negative effects. Use of above-the-knee assistance tube and sleeping with the head of the bed elevated may likewise decrease postural decreases in high blood pressure. The advisable elements of a fall-focused physical exam are displayed in Box 1.
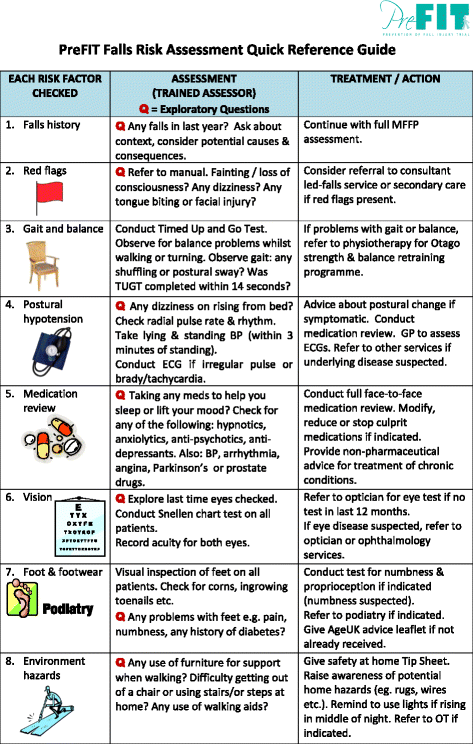
A Yank time greater than or equivalent to 12 secs suggests high autumn threat. Being incapable to stand up from a chair of knee height without utilizing one's arms suggests enhanced autumn threat.
Report this wiki page